Table of Contents
- What are models?
- Biomedical Model:
- BioPsychoSocial Model:
- Important research studies:
- Sample Questions:
Welcome to the thrilling world of Health Psychology, where we will be diving into the world of models! No, we’re not talking about the ones that strut in fashion shows (one can dream), but the ones that shape our understanding of health. These aren’t your average, everyday models – they dont pose for pictures; they pose for questions about our well-being.

What are models?
In science, a model is a theoretical framework that helps us to understand real-world complex systems. These models can be mathematical, visual, or in this case, psychological. Some examples of psychological models include the multi-store memory model (Atkinson and Shiffrin) and the Working Memory Model (Baddeley and Hitch), which attempt to show visual representations of a complex process: memory.
Check out our blog about the models of memory here!
There are 2 models of health:
- Biomedical model
- Biopsychosocial model
Biomedical Model:
Let’s dive in to the first model! The biomedical model is like the Sherlock Holmes of health psychology. It’s all about the evidence and clues as to why our bodies drop like breadcrumbs, leading us (detectives) to the ‘whodunnit’ of illness. It’s a model that aims to uncover the truths hidden in the nooks and crannies of our biological being.
But in all seriousness, at it’s core, the biomedical model of health zeroes in on biological mechanisms as the primary drivers of diesease and behavioural patterns regarding health. However, this perspective doesn’t take into account for the various social and cognitive factors – environment, socio-economic status, decision making – that also play important roles in health and wellness. The model operates under the main assumption that various biological factors such as biochemical imbalances and neurological abnormalities, are the sole culprits behind illnesses.
It’s essentially saying that the brain is the only determinant of your psychology and your mental self and bein; the mind is exists only as a result of the brain. Due to this, it’s known as a reductionist model, as it explains complex phenomena from a simple biological approach. The model, however, was very effective in treating physical illnesses and had been known as the dominant model for dignosing and treating illnesses. This meant that helath campaigns and treatments were limited to biological treaments and solutions, ignoring sociocultural and psychological causes and treatments entirely.

BioPsychoSocial Model:
If the biomedical model is the meticulous mechanic of health, the biopsychosocial model is the ultimate party planner, mixing biological ingredients with a psychological punch and a sprinkle of social spice (6th member of the Spice Girls?). It doesnt just listen to your heartbeat, it wants to know about your last heartbreak and how many friends you have on social media. So let’s dive into the biopsychosocial model, where every aspect of your life is on the guest list for the grand gala of health!
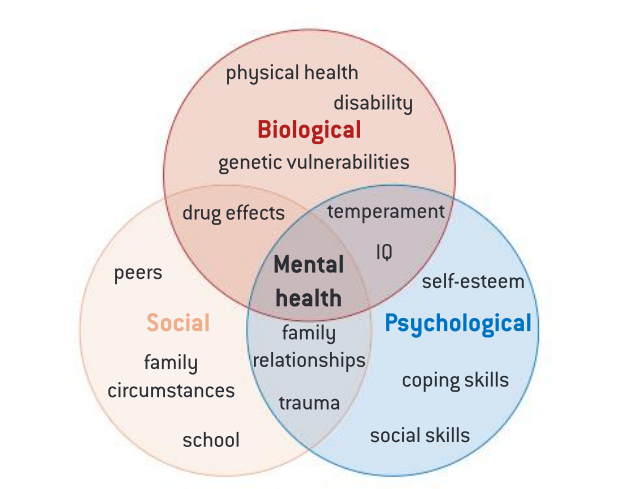
The model was developed by Engel (1977) and it’s main arguement is that there is a lot more to health and wellness than simple biology. People’s health depends on a number of things known as ‘determinants of health’. These determinants encompass everything including someone’s social and physical environment, access ot health services and individual behaviour as well as biology and genetics. The BPS model reaches far beyond the biomedical model aand ackknowledges the complexity of health-related behaviour and wellness.
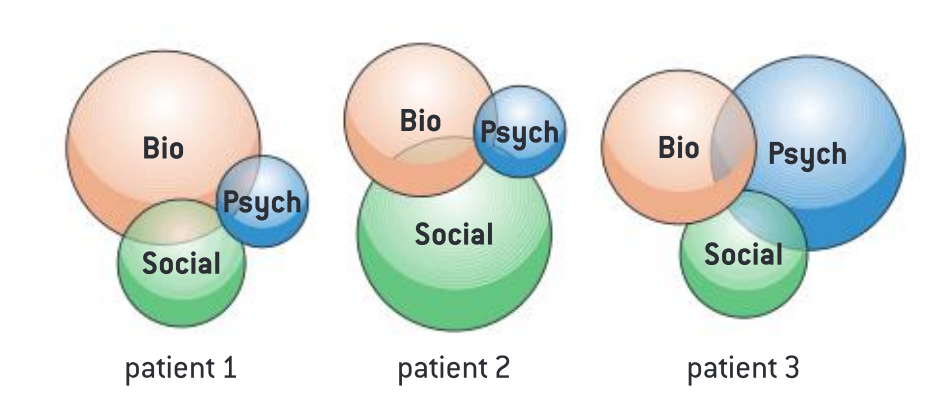
The BPS model is less reductionist than the biomedical model and therefore accounts for more variables, allowing for more holistic explanations of behaviour. However, the model may imply that all three levels of approaches are always important when determining illness, but the relative contributions of each approach don’t seem to be considered. In fact, it is possible that some behaviours or health problems can be treated successfully with only one or 2 components of the model.
Important research studies:
Nguyen et al (2016):
- Aim: To investigate the effectiveness of a treatment programme designed based on the BPS model.
- Method: Retrospective data review
- Procedure and Participants: 142 patients with a mean age of 40 years were recruited for the study, whose avergae weight at the start of the study was 210.2 lbs (95.3 kg)
- The programme combined the medical knowledge of insulin with cognitive behavioural therapy (to reframe thinking) and behavioural therapy (to break unhealthy eating habits.
- Participants were taught about insulin and its role in fat storage.
- They studied the food groups that affect insulin and were advised to limit the intake of these products in order to keep insulin low.
- Phentermine—a drug that suppresses appetite while maintaining energy and alertness—was prescribed to participants
- CBT techniques were also incorporated into the programme to help participants change their thinking patterns.
- Participants were asked to follow an eating schedule with five meals a day. They were instructed never to starve themselves, but to avoid sweets and artificial sweeteners.
- Behavioural interventions were aimed at breaking old eating habits and developing new ones.
- Results:
- There was a 10.8% decrease in weight on average from the baseline to completing the programme over 86 days
- from 210.2 lbs to 187.4 lbs; 95.3 kg to 85.0 kg
- Over the same time, BMI decreased from 34.6 to 30.1
- Strengths:
- Large sample size – increases validity of the results -> can be applied to other treatment programs
- The use of cognitive behavioural therapy and insulin knowledge and appetite suppressents – good treatment strategy
- Holistic approach to obesity treatment – biological, social, and psychological factors and determinants
- Limitations:
- Lack of a control group -> Can’t solely attribute results to the BPS model
- Short treatment duration -> long term effects were not assessed
- Retrospective nature -> limitations in data accuracy
- Ethical considerations: No major ethical considerations!
Cohen et al (2003):
- Aim: To explore the treatment of nicotine dependance using a biopsychosocial framework.
- Method: comprehensive literature review -> meta analysis
- Participants and Procedure: The researchers reviewed and synthesizes findings from various studies to understand the multifaceted (complex) nature of nicotine addiction and its treatment.
- Results: The analysis showed:
- Chronic use of tobacco products is one of the most preventable causes of death and illness, specifically in the US, with more than 430,000 individuals dying each year due to tobacco-related diseases.
- Tobacco use is associated with a range of ilnesses, including various cancers, cardiovascular disease, etc.
- Despite public health efforts, the prevelance rates of tobacco use have not significantly changed, and in some demographics, they have increased.
- Nicotine dependance and the process of smoking are best understood through the biopsychosocial lens.
- Strengths:
- Meta analysis -> comprehensive review -> large data sample -> increases the validity of the results
- Limitations:
- No new data was obtained for the study -> The study is just commenting on previously documented results and trends.
- Ethical considerations: No major ethical considerations!
Sample Questions:
Q. Evaluate the biopsychosocial model of health and well-being. [22]
- Introduction:
- Start with a general introduction to health and health psychology
- Follow up with a brief explanation of health models
- Next, write a breif introduction into the biomedical model (for context)
- Biopsychosocial model:
- Since this is a 22 mark question, you will have to describe the model in detail
- Start with introducing the model and who developed it (Engel, 1977)
- Then introduce each component of the model and explain them (biological, psychological, social)
- Since the question asks to “evaluate” the model, it is also recommended that you consider these important points:
- The importance of the model in understanding and considering a holistic appraoch to health
- Advantages and disadvantage of the model -> limitations of the model can also be discussed
- Supporting research:
- Study 1 (aim, method, participants and procedure, results, strengths, limitations, ethical considerations)
- Study 2 (aim, method, participants and procedure, results, strengths, limitations, ethical considerations)
- Conclusion:
- Refer back to the introduction and discuss how these 2 studies have supported your claims
- Connect the whole thing to the bigger picture of health psychology in its practical applications.
And that brings us to the conclusion of this blog! Now all we can do is pray to get a 7 in psychology!
Check out our other psychology related blogs here.
Sources: